It was the middle of July when Sandpoint resident Joe Jarzabek, 65, and his wife began to feel ill.
“My wife went through the drive through testing center in Sandpoint,” he said. “We didn’t get results right away, but when we got her result, it was positive.”
He said he knew then they were both sick with COVID-19, the disease caused by the novel coronavirus SARS-CoV-2.

A week after his symptoms began his condition worsened. “I was coughing so hard … it felt like I couldn’t breathe,” he said. Jarzebek and his wife went to Bonner General Health’s emergency department.
After physician assessment, Jarzabek was transferred by ambulance and admitted to Kootenai Health’s COVID-19 isolation unit to receive critical-level care.
“They were so professional,” Jarzabek said. “I was really messed up. I had trouble breathing and they put me in intensive care. I don’t remember much of the first five days.”
As of August 23, Jarzabek had been a patient at Kootenai Health for 30 days on the COVID-19 isolation unit. He has since been discharged.

“The thing that impressed me is that this facility, the COVID-19 isolation unit, came together so fast. The fact that they were able to put something like this together in such a short time; it’s incredible,” he said.
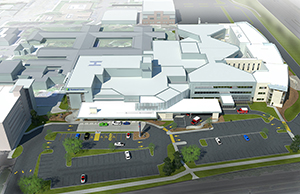
The third floor of Kootenai Health’s east wing expansion opened this past November for oncology and neurology patients before being transformed into the hospital’s COVID-19 isolation unit on July 30. As an isolation unit for COVID-19 positive patients, the floor is locked to all but essential employees who wear personal protective equipment like masks, gowns, gloves, and eye wear continuously. They change gloves with each patient.
The unit features special donning (putting on) and doffing (taking off) areas for staff to get ready for, and leave after, their shifts.
“I haven’t left this room since I was transferred from the ICU,” Jarzabek said. “No one from outside is allowed in. That can be hard.”
But he says the spacious room and the view helps.

“It’s a real advantage to northern Idaho to have this facility,” he said. “There were a couple of times I needed scans right away and they had all the equipment ready at a moment’s notice. Because of how they are organized with their treatment — everyone knows what everyone else is doing.”
“I can’t say enough about the care,” he said. “They helped me not just with the physical side of things, but with the mental.”
He said his former nurses on the unit will come and check on him, even if he’s not their patient for the day.
Jarzabek doesn’t know how he contracted the virus. Since news of the pandemic broke he and his wife were diligent in wearing masks and social distancing. Self-described homebodies, they rarely left the house and if they did need groceries, his wife went at off times and wore a mask religiously.
Jarzabek has spent most of his life in Sandpoint as a personal injury attorney, now retired. He and his wife just celebrated 40 years of marriage. He said he has never been an inpatient in a hospital before and has had low blood pressure his whole life.

He said the current debate about mask wearing has discouraged him. “There’s no conspiracy,” he said as his heart rate monitor beeped faster, showing his passion for the topic. “There’s nothing I can take that is going to make this leave tomorrow. It attacks everything — the thickness of your blood, it goes after your heart; basically any organ. My lungs are filled with fluid — they are white. It’s a difficult disease and there is no cut and dry treatment. If I try to walk three to four steps, I will be out of breath. My nurse told me, ‘it takes time, and time takes time.’”
“We should be working together as a community. If you can just treat people with respect and understand you can save someone’s life,” he said. “I wouldn’t wish this on anyone. It can be mild. Or you can be here going on 30 days.”
To view more photos from Joe’s experience, view our COVID-19 photo gallery.